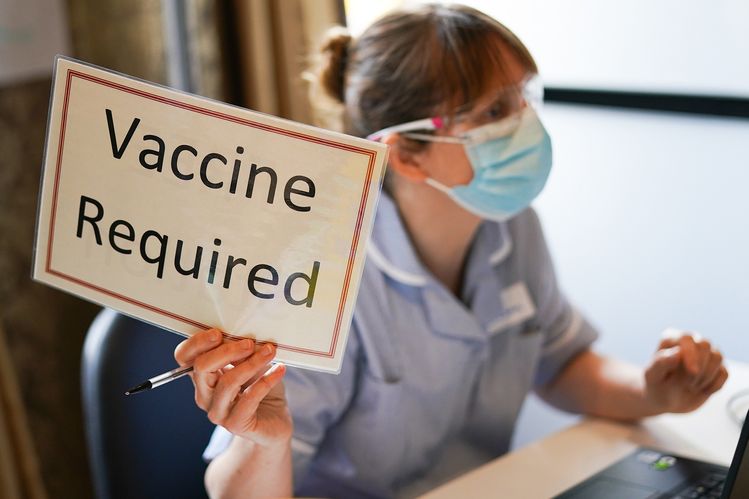
But when 18 October arrived, 95% of staff had met the requirement through vaccination or an approved exemption. (The other 5%, including partially vaccinated staff, are currently on administrative leave.)
Charleen Tachibana, an executive who has spent her entire career at Virginia Mason, believes that this high vaccination rate is partly because “we have a long history of [a] vaccination requirement… it’s pretty well been normalized”.
Back in 2004, Virginia Mason reportedly became the first medical center to require all of its staff to be vaccinated against influenza each year. The administration held focus groups and other activities, including quizzes and a party, to encourage discussion of the new requirement. The combined carrot-and-stick approach proved very successful, and the influenza vaccination rate of Virginia Mason staff shot up from 54% to 98% in two years.
The lessons learned from that experience informed the rollout of the coronavirus vaccine requirement. One aspect was ensuring that it was as convenient for staff to receive the jabs as possible. The other aspect was a heavy focus on communication around the new requirement, including information sessions and documents in multiple languages.
“We don’t take mandates lightly,” says Tachibana. “When there’s such clear science to this – when the vaccine has been proven to be safe and highly, highly effective – we’ve moved forward with these.”
As Virginia Mason’s experience suggests, a vaccine mandate is a powerful tool for safeguarding public health. But it can also be a highly contested one. In some ways, attitudes towards the current Covid-19 vaccine requirements reflect the patterns of previous centuries, making it important to understand the historical lessons of compulsory vaccination.
Precedents for vaccine mandates
In the 17th Century, Chinese physicians found that when cowpox was applied to a wound, it could lead to immunity against a more dangerous infection: smallpox. As the technique spread around the globe, eventually some leaders mandated this kind of inoculation. For example, during the American Revolutionary War, in 1777, general George Washington required all troops to be inoculated against smallpox.
Inoculation gave way to more sophisticated vaccination once the English doctor Edward Jenner developed a smallpox vaccine in 1796. Mandatory vaccination began just a few years later. In 1806, Elisa Bonaparte, the ruler of Lucca and Piombino in present-day Italy (and sister to Napoleon), mandated the vaccination of newborn babies and adults.
Another milestone occurred in 1853, when the Compulsory Vaccination Act required infants in England and Wales to be vaccinated against smallpox.
Though some vaccines, like for polio, were initially popular, one noticeable pattern is the public getting used to a particular vaccine requirement over time, then some people getting spooked by a novel vaccine.
“The United States has had vaccination mandates in place since the late 1970s,” says Lee Hampton, a paediatrician and medical epidemiologist with Gavi, the Vaccine Alliance. And Italy requires children to be vaccinated against a range of pathogens, such as hepatitis B, diphtheria, pertussis, poliovirus, tetanus, Haemophilus influenzae type b, measles, mumps, rubella and varicella.
According to Hampton, “the mandates themselves… hadn’t really caused any issues. What has caused changes over time in those types of contexts is when what’s being mandated changes.” This pattern has been seen, for example, with new requirements for vaccination against hepatitis B, anthrax and of course now Covid-19.
Vaccination is now required in some cases for school attendance (for example, against hepatitis B in Slovenia), for organ transplants (some parts of the UK require them for kidney transplants) – and in one extreme case in Italy, to retain custody of children. Penalties for non-compliance are most often educational or financial.
Vaccine mandates are especially common in high-income countries, according to Hampton. There also tends to be a link to the style of government, where “the more authoritarian the government, the more likely it is to have vaccination mandates”. This may not be surprising, because it’s easier for this style of government to impose new rules, including those in the public interest (in the case of vaccines).
For instance, The Gambia mandated childhood immunisations in 2007, during a period of authoritarian rule (and following a drop in immunisation coverage). However, mandatory vaccination is also common in democratic countries in emergency situations, such as during pandemics – the US state of New York imposed mandatory flu vaccines on healthcare workers temporarily during the swine flu pandemic in 2009.
The legacies of “conscientious objection”
Over the centuries, some objections have arisen over the components used to make vaccines. Certain vaccines include tiny amounts of animal products, like squalene, an oil from shark livers. The polio vaccine previously used cells from monkey kidneys. These types of ingredients have led to some vegetarian opposition.
The early smallpox vaccine involved cowpox lymph, taken from calf blisters. To parts of the growing vegetarian and anti-vivisectionist movement in Victorian Britain, this was repugnant.
These vaccine objectors had various reasons, according to Sylvia Valentine, who’s currently writing her PhD thesis on the subject at the University of Dundee. “Some of the non-conformist denominations believed the human body should not be contaminated with animal material,” Valentine explains. “The anti-vivisection movement was also involved with anti-vaxxers and many objectors were ‘anti’ lots of other things too, including state interference in their lives. The anti-vivisectionists would have objected to the methods used to produce the calf lymph, which were rather gruesome if I am honest, and were concerned about animal welfare.”
Porcine tissue has also led some Muslims to worry about whether certain vaccines are halal – for instance, if they use pig-derived gelatine as a stabiliser. This challenged measles vaccination in Indonesia in 2018. More recently, Muslim clerics in Indonesia have declared that Covid-19 vaccines are permissible, and Covid-19 vaccine manufacturers have stated that these vaccines do not contain pork products. Some Jewish authorities have also insisted there should be no problems with non-oral vaccines containing pork-derived ingredients.
Another contested component is foetal cell lines following abortions that were performed legally decades ago. These cell lines continue to be used in the testing of some vaccines and the development of others. Regardless, the Vatican has declared coronavirus vaccines “morally acceptable”.
While there will be disagreement between sects and individuals, particularly where religion is highly decentralised – as among US evangelical Christians – there are no established religions that prohibit vaccination.
In fact, throughout history, religious officials have played important roles in encouraging and implementing vaccination. After all, it’s in their interest to safeguard the health of worshippers.
Along with spiritual objectors, a long thread of labour activism has been linked to vaccine opposition. During the Victorian era some English employers imposed smallpox vaccine mandates, which were particularly likely to affect – and especially resisted by – the working class. Labour unions have been important sources of organised opposition (including, in 2004, unionised nurses challenging the influenza vaccine requirement at the Virginia Mason medical centre).
From 1898, England allowed conscientious objections to mandatory vaccinations. However, it wasn’t until 1907 that these exemptions became relatively easy to get – eventually extending to one-quarter of all births.
Though the small minority of anti-vaxxers today are very vocal, “the Victorian anti-vaccination movement was much larger”, believes Nadja Durbach, a historian of the body at the University of Utah. “It was also more mainstream than anti-vaccinationism today. There were more unknowns in terms of the science of vaccination and because of a lack of sanitation, meant that the process could easily lead to infection.”
There continue to be parallels between contemporary and historical vaccine protest. Anti-vaxx effigies even continue to be burned in some places occasionally, such as in Utah, US, in May this year. But one difference is the occasionally carnival-like atmosphere of the Victorian protests. As Durbach has written, “a common anti-vaccination demonstration involved driving a newly-released anti-vaccinationist prisoner, often still in prison garb, around in a cart adorned with ribbons and banners and accompanied by a brass band”.
A push vs. a nudge
Compulsory smallpox vaccination ended in the UK in 1947, amidst a broader trend toward optional vaccination (for example against diphtheria) with a focus on education and persuasion. Yet as we’re seeing now with Covid-19, and as before with smallpox, vaccination mandates do increase uptake. For example, when France mandated 11 childhood vaccinations – against potentially lethal diseases – for those born after 2018, the number of fully vaccinated children increased significantly over previous years.
When chosen carefully, there’s no question that mandatory vaccinations can save lives. For example, one study found that patients were substantially less likely to die (with mortality rates of around 13.6% mortality verses 22.4%) in hospitals where healthcare workers had higher rates of flu vaccination compared to those with low rates, though patients were equally as likely to be infected with the virus.
Another European study also found that in countries with mandatory measles vaccinations, and without non-medical exemptions, the disease incidence was 86% lower than in countries without the mandates.
One common tension is between obligation, which can increase hostility, and voluntary vaccination, which can increase transmission. Some health experts are nervous about mandatory vaccination because these policies may diminish trust in medical authorities over the long term. Vaccine mandates have led to violent riots in Brazil and may have contributed to vociferous anti-vaccine movements all over Europe, for instance.
In France, one of the world’s hotspots of vaccine hesitancy, the Ministry of Health has attempted to reduce the polarising effects of vaccine mandates by embedding mandates within a broader effort to build trust. This has led to improved vaccine coverage, although a significant minority are still vaccine-hesitant – suggesting the importance of continuing to monitor attitudes and strengthening relationships between the medical establishment and the public.
However, not everyone agrees on what counts as a “mandate” – there’s an argument that many so-called mandated vaccinations are not technically mandates because people can usually opt out in certain circumstances, such as on religious grounds. And enforcement can be loose or even non-existent.
Coercive vaccination – which involves enforcing mandatory vaccination through physical force or intimidation – is different. And despite the beneficial effects of increasing vaccine uptake, there’s more of a consensus that this strategy should be avoided. Yet, according to Yaqiu Wang, a China researcher for Human Rights Watch, coercive tactics including harassment and spying are being reported in some parts of China. This isn’t necessarily an official national policy, Wang explains. But the central government issues tough vaccination quotas for local governments, such as the September 2021 guidelines to vaccinate at least 90% of children in China. “This kind of central government quota/decree drives up vaccination rate, but sometimes this can result in coercive vaccinations at the local level,” says Wang.
Even in the absence of physical force, certain penalties for noncompliance with mandates can be counterproductive – for instance, if substantial fees are levied on people who already find it hard to take the time off work or travel to vaccination sites. This was a bone of contention among silkworm growers in the 19th Century and remains an obstacle for some people who have not yet been vaccinated today.
Vaccine mandates are “something to be used sparingly”, with the minimal level of enforcement possible, according to Hampton. The conditions for their use should include “the presence of a life-threatening disease, particularly a highly contagious life-threatening disease, and [a safe and] effective intervention for reducing transmission of that disease. That’s usually a pretty good combination.
“It helps that the vaccines that we have for Covid-19 are on balance really, really safe,” he adds. He remains optimistic that vaccination mandates will continue to be a useful way for protecting populations despite the opposition they face.
“With careful and judicious use, the benefit from using those mandates will outweigh the harms,” he says. Whether that is enough to convince the sceptics, remains to be seen.
-BCC -By Christine Ro